News Letter, Vol. 1 (2)
February, 2009
© Copyright
Jun Xu, M.D. Lic. Acup., Hong Su, C.M.D., Lic. Acup.
www.rmac.yourmd.com
www.drxuacupuncture.co
Rehabilitation Medicine and Acupuncture Center
1171 East Putnam Avenue, Building 1, 2nd Floor
Greenwich, CT 06878
Tel: (203) 637-7720
Case Discussion 2: Intolerable Headache
September 28, 2008
Patient Name: Joan T.

Joan T., a 16-year-old schoolgirl, was brought to me by her mother, because the girl had been suffering from headaches since she was 12 and first had her period. Her headaches were so severe that four or five days of the week during her period she was often not able to go to school. These headaches manifested themselves on both sides of the temporal area and also caused severe pain to the left eye. Because of the severity of the pain, Joan called her mother several days a week to pick her up from school, and the headaches were interfering with her school work. This made it necessary for her mother to quite her job and to begin to home school Joan, which she did for several years. However, at 16, Joan returned to high school as a junior in order to start preparing for the college entrance exams as well as apply to colleges. Her headache pain had become so severe that Joan was sleeping poorly, was extremely stressed, which often resulted in tears and depression, which made her eat too much, causing a large weight gain. Her mother had taken her to all kinds of doctors in hopes of alleviating her condition, but nothing helped, especially the drugs prescribed for Joan’s headaches. Her SAT exams were commencing in two months, at which point the mother finally brought her to me for evaluation.
By physical examination, Joan was a slightly obese young girl, very depressed and stressed. She spoke in a low tone; she did not like light, felt pain by touching her temporal area and back of the scalp, i.e. the occipital area.
The patient might have one of the following three types of primary headache, i.e., tension, cluster, or migraine geadaches. She might as well have a mix of the two or three of the following headaches.
Tension headache: Tension headache is the most common type of chronic and frequent headache. The symptoms include steady pain on both side of the head and or back of the scalp with the feeling of pressure and tightness around head and as if a band was put tightly around it. The pain usually increased over period of hours when the pain gets worse, and might develop pulsating quality. The pain radiates from neck, back, eyes or other body parts.
Cluster headache: Cluster headache is often described as a sharp, penetrating or burning sensation on the one eye. The patients feel as if somebody punched the eye and this pain is of sudden onset without warning; within a few minutes excruciating pain develops and people with cluster headaches appear restless The pain is so severe, some patients report it is even worse than childbirth. The cluster headache usually lasts about 2 to 12 weeks, though some chronic cluster headaches may continue for more than a year. These sometimes go with seasonal change.
Migraine Headache: A migraine headache is a throbbing or pulsating headache that is often one side and associated with nausea and vomiting, and sensitive to light, sound, and smell with sleep disruption and depression. These attacks are very often recurrent and do not change with age, sometimes develop a chronic migraine headache.
There are two subtypes of migraine headache, migraine with aura and migraine without aura. Most auras are visual and are described as bright shining light around objects or at the edges of field of vision or zig‑zag lines with wave image or hallucinations, some may experience temporary vision loss and motor weakness, speech, or language abnormalities, dizziness, vertigo, tingling, or numbness.
A MRI of migraine patient
The causes of headaches are usually different.
The causes of tension headaches are usually caused by stress, muscular tension, and gouty arthritis on the neck or spine,
postural changes, vascular dilatation, protracted coughing or sneezing and fever and depression and temporal mandibular joint disorder etc.
The cause of the cluster headaches is unknown, however, cluster headache also well known to be triggered by alcohol, nitroglycerin, or similar drugs.
The cause of migraine headaches is unknown either. It is very often. There is a family history of disorder and migraine headache can be triggered with many stimulants for example alcohol, weather,
altitude, exertion, food, and color and contrasting pattern, hormonal change, hunger, lack of sleep, medicine, perfume and stress etc.
From the western medicine point of view, there is many different kind or medications to treat headaches. For example, Topamax, Imitrex are using for migraine headaches with some successful cases. However, beta blockers, antiseizure medication, calcium channel blockers, tricyclic antidepressants, and analgesics such as aspirin, ibuprofen, acetaminophen etc are tried to treat migraine, cluster, and tension headaches. However, most of these drugs can not provide significant improvement for above headaches. Therefore, more and more patients are starting to look for alternative treatments. Acupuncture is one of the best therapies for the headaches.
Chinese medicine classifies headaches into two categories:
1.
External wind attack headaches: the headaches are caused by external factors, such as wind cold and wind heat. The headaches usually have a character of acute onset and very severe and constant attack.
Wind Cold: it shows periodic attack, the pain always is connected with neck and upper back and aversion to wind and cold, the head feels heavy, likes to have a band to tight around the head. The patient does not feel thirsty, and have thin and white coating on the tongue with floating pulse.
Wind Heat: feels expending headache from inside of the head, accompanied with fever and aversion to heat and wind, reddish face and eye, feels thirsty, constipation, yellowish urine, red tongue body with yellow coating on the tongue and floating pulse.
2.
Internal organ dysfunction headaches: internal headaches usually are slowly onset and the pain is mild and sometimes feels emptiness within the head. When patients are on stress and overwork, the pain will be worse. The pain is on and off and usually last for long time.
According to traditional Chinese medicine, head is the collection of all the Yang Meridians. The six Yang Meridians all distribute to the head and face and also liver Meridians go up to the top of the head, therefore, headaches can be diagnosed based on the meridian distribution. If we know the Meridians distribution, so then we will be easier to make clear diagnosis and treatment.
1,
Tai Yang (Urinary Bladder) meridian headache usually located at top of the head and back of the head and connected to the neck.
2,
Yang Ming (Large Intestine) meridian headache usually is on front of the head, i.e. the forehead including upper portion of the eye.
3,
Shao Yang (Gall Bladder) meridian headache usually is on the bilateral temporal area and radiates to the ear.
4,
Jue Ying (Liver) meridian headache usually is on the top of the head sometimes connecting to the eyes and frontal head. (Large Intestine) meridian headache
Acupuncture treatment for headaches:
First ask the patient the location of the headache and the severity of the headache, i.e. find out which internal organ shows dysfunction.
Second ask the patient about their accompanied symptom, differentiate the wind cold from the wind heat.



- For Tai Yang (Urinary Bladder) meridian headache, i.e. the headache locates on top of the head and back of neck. We choose the following, GB20 Feng Chi and DU16 Feng Fu and DU19 Hou Ding and BL9 Yu Zhen and BL60 Kun Run and SI3 Hou Xi.

- For Yang Ming ((Large Intestine) meridian headache, i.e. the headache locates on the front of the head, i.e. the forehead including upper portion of the eye. The acupuncture points are Yin Tang and Tai Yang (Extraordinary Points), Lu 7 Lie Que, LI 4 He Gu, GB 14 Yang Bai
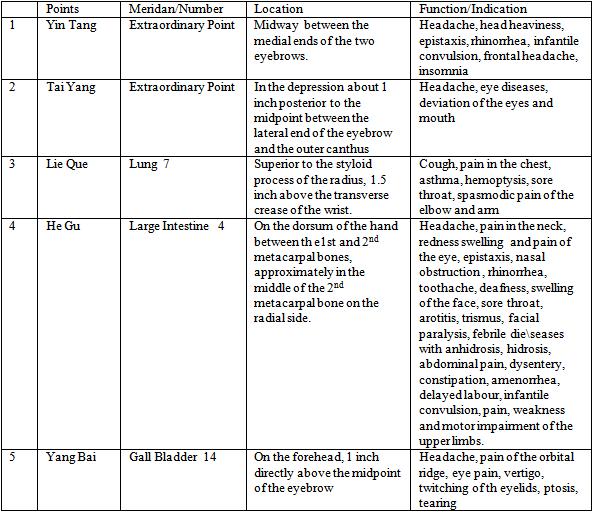
- For Shao Yang (Gall Bladder) meridian headache, i.e. the headache usually is on the bilateral temporal area and radiates to the ear. The following points are chosen, GB 20 Feng Chi, Extra Point 1 Tai Yang, SJ 5 Wai Guan, ST 8 Tao Wei, GB 38 Yang Fu, GB 39 Jue Gu.

- For Jue Ying (Liver) meridian headache usually the pain is on the top of the headand many time it connects to theeyes and frontal head. Du 20 Bai Hui, Liv 3 Tai Chong, Lung 7 Lie Que.

If the patient with above symptoms accompanied with the wind cold or wind heat signs, we will add the following points:
- Wind Cold: GB 20 Feng Chi, Extra Point Tai Yang , ST 8 Tou Wei, GB 8 Shuai Gu, UB 12 Feng Meng, UB 60 Kun Lun.

- Wind Heat: GB 20 Feng Chi, Tai Yang, St 8 Tou Wei, GB 8 Shuai Gu, Du 14 Da Zhui, SJ 5 Wai Guan,

Personal tips for clinical use:
Acupressure tips for patients:
- If you have headache, please differentiate the site of the headache, i.e. identify if you have Tai Yang, Yang Ming, Shao Yang, or Jue Ying headache.
- After you identify the site of the headache, then try to locate the points by following the above tables and pictures.
- Acupressure the points with your knuckle, press with the comfortable pressure on the points, count 20 counts then change to another points. You should use the symmetric points at the same time.
- Your acupressure points mainly locate on the head, use the head points as the major acupressure points. You may ask your friends or family members to help you with moderate acupressure.
Acupuncture Tips for Practitioners:
- The most important is to identify which meridian headache your patient belongs to, i.e. Tai Yang, Yang Ming, Shao Yang, or Jue Ying.
- Identify the external type, i.e. wind cold or wind heat. If you could combine the meridian with the external type, your acupuncture effects will be much more than the average acupuncturists.
- The distal points, i.e. on the hands and feet, are very important for your treatment. Please do not ignore the distal points.
- Please put your patients in a quite and low illuminated room, with electrical stimulation for 30 min.
5. Many headaches may be triggered by occipital neuralgia, trigeminal neuralgia, common cold, sinusitis and allergy etc. For those headaches secondary to the above, we have to treat the original trigger. We should treat the sinusitis, occipital neuralgia, trigeminal neuralgia, common cold, allergy, etc. If we can effectively treat the original trigger of the primary headache, our patient’s recovery rate will be much higher the average of acupuncturists. For many years, 99% of my patients felt much improved after my treatment because I notonly treat the symptom of headache, but I also treat the trigger factors.
Joan’s headache is very complicated. From the western medicine point of view, her headache belongs to migraine headache. However, her headache always triggered by occipital neuralgia and worsen with her hormone and menstruation. Every time when she has hormonal change and also sometimes occipital nerve pain, her headache symptom would get worse. Therefore, she has four to five attacks per week.
After I made a clear diagnosis, first I used GB20, DU16, and Bai Hui and also Tai Yang, and LI4. The patient underwent my treatment three times a week for about two months and she also was injected with cortisone to block her left and right occipital nerve pain, her headache is much-much better. After my treatment, the patient took her SAT test and applied for college, she was accepted into the Boston College and after two years follow up, her mother reported that Joan is great and she has no any major headache attack. She survived her college study. Her mother is very-very thankful to me.

One comment
Pingback: Case Discussion 6: Bronchitis « Dr. Xu Acupuncture