News Letter, Vol. 2 (12), December, 2010, © Copyright
Jun Xu, M.D. Lic. Acup., Hong Su, C.M.D., Lic. Acup.
Robert Blizzard III, DPT
Rehabilitation Medicine and Acupuncture Center
1171 East Putnam Avenue, Building 1, 2nd Floor
Greenwich, CT 06878
Tel: (203) 637-7720
Dear Friends and Patients:
Happy Holidays!
This is the last newsletter for 2010. We are very happy to introduce Dr. Robert Blizzard, who recently joined in our practice. Dr. Blizzard graduated from the University of Connecticut with a Bachelor’s Degree in Exercise Science, and continued on to receive his Doctoral of Physical Therapy at Franklin Pearce University. He is a full time licensed physical therapist in RMAC. We believe his knowledge and experience will help you to fulfill your goal to be completely recovered from your injury. Dr. Blizzard joined us to write this newsletter too.
From now on, we will leave our comment space on under the news letter at our website, www.DrXuAcupuncture.com. you are welcome to leave your questions or comments . We will try our best to answer your questions.
We wish you happy holidays!
Jun Xu, M.D.
Hong Su, C. M. D.
Robert Blizzard III, D.P.T.
Low back pain with failed back surgery syndrome (FBSS)
From: www.yorkshirehighlanders.co.uk
Peter is a 56-year-old male who complains of low back pain for three years. The pain started from the low back and radiated down to the right leg, which made it difficult sitting, walking, and standing. The pain also interferes with his sleep, especially while he changes positions in the bed, and therefore he went to his primary care physician. He was referred to physical therapy for about three months of treatment. However, the pain was not getting better and still he felt pain is sharp and stabbing, and that radiated down to the right lateral thigh and the lower leg. The pain was constant. In the meanwhile, he gradually felt his leg was weak and he had difficulty standing from the sitting and driving position.
Then one day he realized his underwear was wet because he had difficultly controlling his urinary bladder and he had decreased sensation at right lateral lower leg. Therefore, his primary care physician referred him to a neurosurgeon. An MRI was done, which showed two large right L4/L5 and L5/S1 herniated disc with impingement of right L5, S1 nerve roots. He was advised to have surgery, L5/S1discectomy.
However, he was afraid of the surgery, then he consulted another neurosurgeon, who suggested to have laminectomy because the MRI, which showed two levels, L5 and S1, with severe right foraminal L5-S1 nerve impingement and degenerative changes between L5 and S1 and S1 and S2, which are the reasons for urinary incontinence.
He was thinking, however, he would like to wait a few more months to see if this would be getting better. He restarted physical therapy again, and also he had epidural injection at those two levels and his pain seemed better slightly. However, he felt the right leg is weaker, he sometimes loses control of his urine. Therefore, he decided to have surgery.
Laminectomy was performed one year ago. After the surgery within one month, he had immediate pain relief and also he could control his urine and the bowel movement. The patient was very happy about the surgery.
However, after six months, he started to feel low back pain again and this time he felt the pain is a gradual onset, dull and achy without any radiating down to the leg and he had no bowel or bladder abnormalities, but he still feels some weakness and mild numbness and tingling sensation on the right lateral leg. He visited his neurosurgeon, who told him this pain sometimes occurred after surgery about 6 months, and if he continued to do the physical therapy, the pain should be getting better.
The patient started to do physical therapy again after six months and he did muscle strengthening and stretching on the low back. However, one day, he felt the pain suddenly getting worse after waking up and the pain is like stabbing with burning sensation around the L3-L4, L5-S1 middle spine and paraspine, and since then, he has had difficulty bending forward and backward, sitting to standing, and driving. The patient then revisited his surgeon and he was prescribed Tylenol with Codeine. After he took this pain medication, he felt better. However, he started to feel drowsy and he had difficulty driving and concentrating on his work, and gradually he also started craving for this drug. If he did not take for one day, he felt uncomfortable not only in the low back but the entire body and also he felt depressed and low energy. Therefore, he came to me for evaluation and treatment.
I performed physical examination, I saw the scars on the both sides of the L4, L5, and S1 para-spine, by palpation, there was tenderness around L3-L4 and L5-S1 para-spine. There was no palpation pain at bilateral sciatic areas. He can bend his low back forward only about 40 degrees and bend his back backward only about 10 degrees. He had no problem to walk on tippy toes and heels. He had no decreased sensation at both legs. I compared the MRI of presurgery and postsurgery, There was no impingement of the nerve roots anymore. Based on all the above information, I thought the patient was suffering with post-lumbosacral laminectomy syndrome, also called “failed back surgery syndrome” (FBSS), refers to chronic back and/or leg pain that occurs after back (spinal) surgery.
Before I introduce the Failed Back Surgery Syndrome, I would like to let you understand the basic knowledge of low back surgery;
There are seven types of low back surgery.
1. Discectomy.
2. Foraminotomy.
3. Intradiscal electrothermal therapy.
4. Nucleoplasty.
5. Radiofrequency lesioning.
6. Spinal fusion
7. Spinal laminectomy, etc.
Discectomy
This is a procedure done to relieve pressure on a nerve root that’s being compressed by a bulging disc or bone spur. In order to relieve this pressure, the surgeon removes a small piece of the lamina (the bony roof of the spinal canal) from above the obstruction.
Figure 24.1
http://indiahealthtour.com/treatments/spine-surgery/endoscopic-micro-discectomy-surgery.html
Foraminotomy
This is type of surgery is undertaken to enlarge the foramen (the bony hole) where a nerve root branches out from the spinal canal. Joints thickened with age, or bulging discs, may cause the foramen to narrow, thereby pressing on the nerve. This pressure can cause pain, numbness or weakness in the extremities. In order to relieve the pressure, the surgeon removes small pieces of bone over the nerve through a small slit, which allows her to cut away the blockage.
Figure 24.2
From: http://www.laser-spine.com/spinehealth/treatments/endoscopic_foraminotomy/
IntraDiscal Electrothermal Therapy (IDET)
IDET is used to treat pain caused by a cracked or bulging spinal disc. This therapy involves inserting a special needle into the disc via a catheter. Once inserted, the needle is heated to a high temperature for approximately twenty minutes, effectively thickening and sealing the disc wall. This procedure reduces inner disc bulge and spinal nerve irritation.
Figure 24.3
From: http://www.advanced-pain-care.com/Intradiscal.htm
Nucleoplasty
Nucleoplasty is used to treat lower back pain resulting from mildly herniated or contained discs. During this procedure, a wand-like instrument is guided by x-ray imaging and inserted through a needle into the disc in order to create a channel. This facilitates the removal of inner disc material. Several channels may be made, depending on the amount of material needing to be removed. After removal, the wand heats and shrinks the tissue of the disc wall in order to seal it.
Figure 24.4
From: http://www.kcpain.com/kcp_help5c.php
Radiofrequency (RF) Lesioning
This procedure is used to interrupt of nerve conduction and the transfer of pain signals. Electrical impulses are used in order to destroy the nerves located in the affected area. A special needle is inserted into the localized nerve tissue, with the guidance of an x-ray. This area is then heated for 90 to 120 seconds, destroying the nerve tissue. This may result in cessation of pain for 6-12 months.
Figure 24.5
From: bnsmedical.com
Spinal fusion
Spinal fusion is a procedure which is done in order to support a weak spine and/or to prevent painful movements. However, spinal fusion requires a long recovery period, and may result in a permanent loss of spinal flexibility. The procedure involves the removal of the spinal disc between two vertebrae, and the subsequent fusion of those vertebrae. Methods of fusion include either bone grafting and/or using metal devices secured by screws.
Figure 24.6

From: http://skillbuilders.patientsites.com/Injuries-Conditions/Lower-Back/Lower-Back-Issues/Lumbar-Spinal-Stenosis/a~51/article.html
Spinal Laminectomy
This procedure is used to relieve pressure on the spinal cord and nerve roots. Also known as spinal decompression, this type of surgery involves the removal of the lamina to increase the size of the spinal canal.
Figure 24.7
 http://www.eorthopod.com/content/lumbar-laminectomy
http://www.eorthopod.com/content/lumbar-laminectomy
Treatments for Faild Back Surgery Syndrome (FBSS)
In 1992, Turner et al. published a survey of 74 journal articles which reported the results after decompression for spinal stenosis. Good to excellent results were on average reported by 64% of the patients. (Turner, J., et al., Spine 1992; 17:1-8 ) Therefore, there are about 36% of the post back surgical patients, who might suffer some degrees of back pain, usually after 6 months of surgery. For some patients, the pain might achieve the peak intensity as pre-operation after two-year surgery.
Failed back surgery syndrome (FBSS), is characterized by intractable diffuse, dull and aching pain or sharp, pricking, and stabbing pain in the back and/or legs accompanied with varying degrees of functional incapacitation. Recurrent herniated disc and symptomatic hypertrophic scar can produce similar low back symptoms and radiculopathy as before the surgery. Gradually increasing symptoms beginning a year or more after discectomy are considered more likely a result of scar radiculopathy, while a more abrupt onset at any interval after surgery is more likely due to recurrent herniated disc. Multiple factors can contribute to the onset or development of FBS, such as residual or recurrent disc herniation, persistent post-operative pressure on a spinal nerve, altered joint mobility, joint hypermobility with instability, scar tissue (fibrosis), depression, anxiety, sleeplessness and spinal muscular deconditioning.
The treatments of Failed back surgery syndrome (FBSS), include physical therapy, acupuncture, minor nerve blocks, transcutaneous electrical nerve stimulation (TENS), behavioral medicine, non-steroidal anti-inflammatory (NSAID) medications, membrane stabilizers, antidepressants, and intrathecal morphine pump. Use of epidural steroid injections may be minimally helpful in some cases. Here, we will mainly introduce physical therapy, pain medications and acupuncture treatment.
1. Physical therapy:
Spine surgery changes the anatomy of the spine but does nothing to improve activation of deep core stabilizing muscles. That is one of the benefits of physical therapy for re-training the body to properly activate the deep core muscles that stabilize the spine. The two deep co-stabilizing muscles of the spine are the Transverse Abdominis (TrA) and Multifidus
Spinal braces are an option to wear especially immediately following surgery to improve recovery. A corset helps to brace the lumbar spine by increasing the pressure in the abdomen, and thus reducing the amount of weight placed through the spine.
Figure 24.8 The Transverse Abdominis is often called the “human corset” as it is the only abdominal muscle attaching to the posterior spine and runs transverse around the body.
The Transverse Abdominis is often called the “human corset” as it is the only abdominal muscle attaching to the posterior spine and runs transverse around the body.
http://www.unm.edu/~lkravitz/Media/transverse.gif http://www.exerciseyourpainaway.co.uk/muscles.htm
Draw-Ins
These exercises can be performed in any position and progressed once the very important concept of TrA activation is achieved. The two starting positions are quadruped and supine. Stabilizing the spine by activating TrA and Multifidus occurs without rotating the hips, tensing the shoulders or holding ones breath but from slowly drawing-in the deep core muscles of the abdominal wall.
Figure 24.10 http://www.strattonpt.com/images/uploads/images.3.jpg
http://www.strattonpt.com/images/uploads/images.3.jpg
http://staceyspt.com/Exercise/LowerBack.htm
Figure 24.12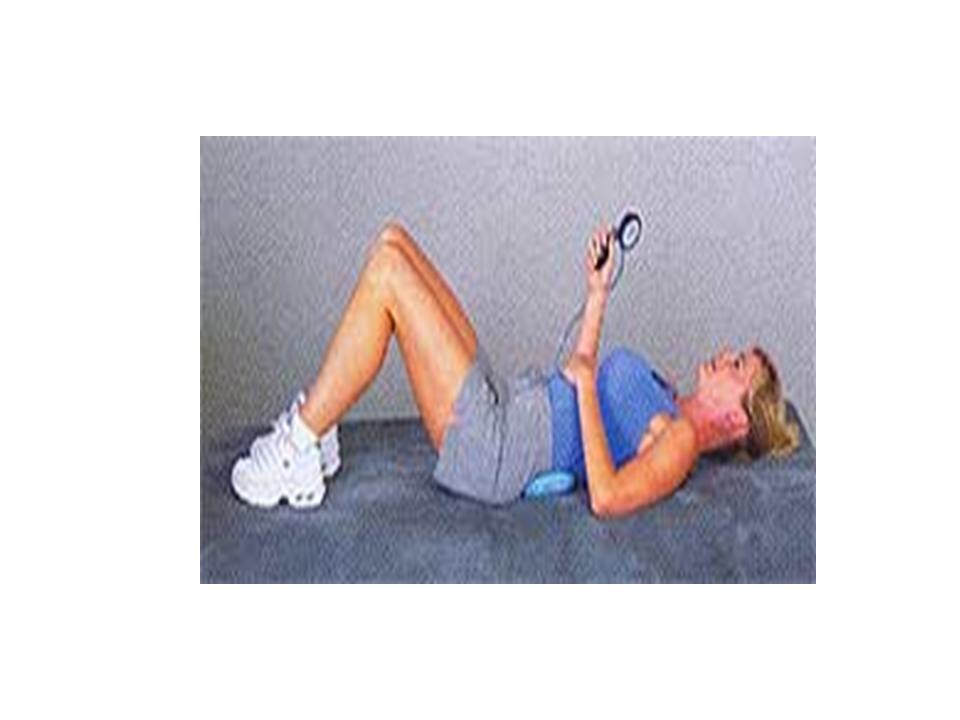 http://www.sportstek.net/pressure_biofeedback.htm
http://www.sportstek.net/pressure_biofeedback.htm
Draw-Ins with Alternating Upper Extremity/Lower Extremity Movement
These movements build upon a solid foundation of spinal stabilization from the previous exercises. Start off first by performing a Draw-In and holding that contraction while moving the Upper Extremities (UE) only, then work on the Lower Extremities (LE) finally moving on to simultaneous movement of both UE/LE. Quadruped Alternating UE/LE Movement is also called “Bird-Dog” while “Dead-Bug” is the name of Supine Alternating UE/LE Movement. It is important to maintain a neutral spine from hips to shoulders and for the core to take in the force when an extremity is lifted and not involve a rotation component to the opposite hand or knee. This will occur if done improperly or rushed to without developing strength and control through the previous mentioned exercises. Both the Bird-Dog and Dead-Bug can be progressed from a solid stable surface such as the ground or exercise mat to an unstable surface such as foam dyna-discs or a foam roller to increase the activation of core stabilizing muscles thus making the exercise more challenging and effective.
Figure 24.13 Bird-Dog Figure 24.14 Dead-Bug
Figure 24.14 Dead-Bug http://michaelwoodspg.blogspot.com/ http://www.canada.com/health/3390881.bin
http://michaelwoodspg.blogspot.com/ http://www.canada.com/health/3390881.bin
Kneeling and Standing Chops/Lifts
Once properly able to stabilize the spine with Alternating UE/LE Movements, progression to more functional activities is deemed ready. Theses moves involve working through all planes of movement while stabilizing the spine.
A resistance cable is used with the hands at arms length from the body starting over one shoulder and working diagonally across the body to the opposite knee, engaging the TrA and keeping from rounding the back forward. In a Cable Lift the hands start at the knee and work diagonally up to the opposite shoulder.
Cable Chops
http://www.menshealth.com.sg/fitness/best-exercises-your-core
Cable Lifts from Kneeling and Standing
http://eas.com/training/strength/rotational-lift–split-squat-cable http://www.whatsupusana.com/2009/04/pregnancy-and-exercise.html
Soft-Tissue Mobilization
Adhesions and scar tissue development are very common following any surgery. Development of these adhesions can lead to decreased mobility and compression on nerve roots causing increased stiffness and pain. A few simple techniques to rid adhesions/trigger points/scar tissue and improve recovery along the spine are from using a foam roller or having manual work specific to your individual needs.
http://www.foamroller.co.uk/ http://www.boulderbodyworks.com/physical-therapy.html
2. Medications:
A. Acetaminoph: (one brand name: Tylenol) helps many kinds of chronic pain.
B. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Examples include aspirin, ibuprofen (two brand names: Motrin, Advil) and naproxen (one brand name: Aleve). NSAIDs come in both over-the-counter and prescription forms. These medicines can be taken just when you need them, or they can be taken every day. When these medicines are taken regularly, they build up in the blood to levels that fight the pain of inflammation (swelling) and also give general pain relief. Please remember that you always take it with food or milk because the most common side effects are related to the stomach.
C. Narcotics: Narcotics can be addictive. For many people who have severe chronic pain, these drugs are an important part of their therapy. If your doctor prescribes narcotics for your pain, be sure to carefully follow his or her directions. Tell your doctor if you are uncomfortable with the changes that may go along with taking these medicines, such as the inability to concentrate or think clearly. Do not drive or operate heavy machinery when taking these medicines.
When you’re taking narcotics, it’s important to remember that there is a difference between “physical dependence” and “psychological addiction.”
Physical dependence on a medicine means that your body gets used to that medicine and needs it in order to work properly.
Psychological addiction is the desire to use a drug whether or not it’s needed to relieve pain. Narcotic drugs often cause constipation (difficulty having bowel movements). If you are taking a narcotic medicine, it’s important to drink at least 6 to 8 glasses of water every day. Try to eat 2 to 4 servings of fresh fruits and 3 to 5 servings of vegetables every day.
C. Other medicines
Many drugs that are used to treat other illnesses can also treat pain. For example, carbamazepine ( Neurotin )is a seizure medicine that can also treat some kinds of pain. Amitriptyline is an antidepressant that can also help with chronic pain. It can take several weeks before these medicines begin to work well.
3. Acupuncture Treatment:
There are three types of Failed back surgery syndrome (FBSS) according to Traditional Chinese Medicine.
Type 1: Coldness and Wetness of FBSS:
Patients feel cold, heavy, and pain at entire low back, difficulty turning over on the bed or standing up from sitting position, getting worse during the cold weather, stiffness at low back, hip and knee joints.
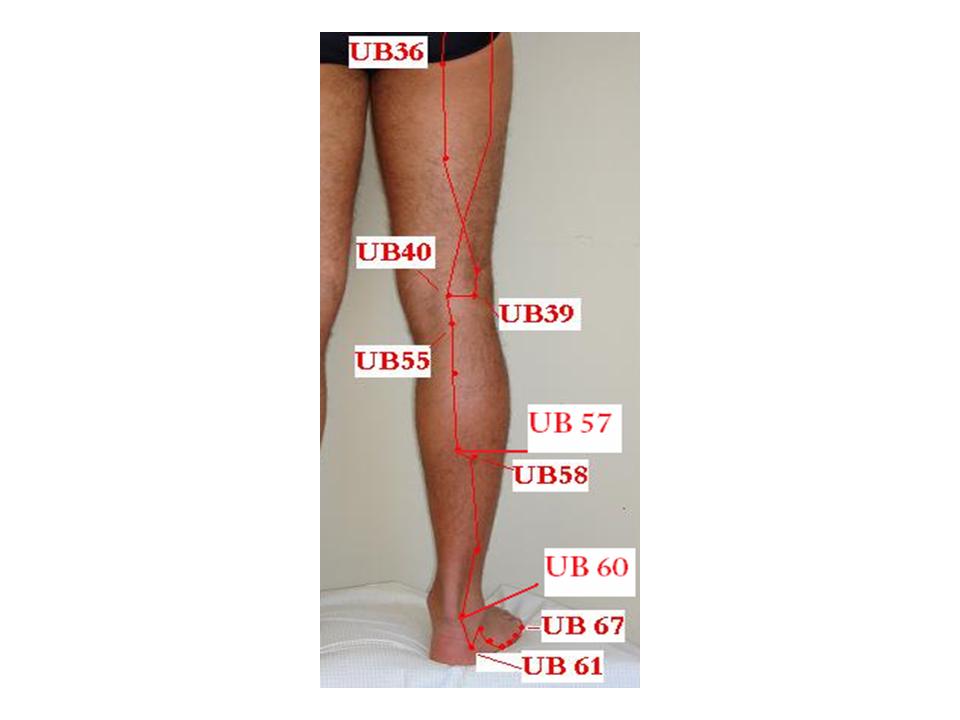
Acupuncture points: UB 25 Da Chang Shu, GB 30 Huan Tiao, UB 40 Wei Zhong, UB 60 Kun Lun, plus Du 26 Ren Zhong, GB 34 Yang Ling Quan, and UB 58 Fei Yang.
Table 24.1
| Points | Meridan/No. | Location | Function/Indication | |
| 1. | Da ChangShu | UB 25 | 1.5 inch lateral to midline of the body on the back, at the level of the spinous process of the fourth lumbar vertebraFigure 24.20 | Low back pain, abdominal distension, diarrhea, constipation, muscular atrophy, pain, numbness and weakness at legs, sciatica |
| 2. | Huan Tiao | GB30 | At the junction of the lateral 1/3 and medial 2/3 of the distance between the great trochanter and the hiatus of the sacrum.Figure 24.23 | Low back pain, thigh pain, muscular atrophy of the lower limbs, hemiplegia |
| 3 | Wei Zhong | UB 40 | Mid point of the transverse crease of the popliteal fossa, between the tendons of biceps femoris and semitendinosius musclesFigure 24.23 | Low back pain, motor impairment of t he hip joint, contracture of the tendons in the popliteal fossa, muscular atrophy, pain, numbness and motor impairment of the lower extremities, hemiplegia, abdominal pain,k vomiting, diarrhea, erysipelas. |
| 4 | Kun Lun | UB 60 | In the depression between the external malleolus and calcaneus tendonFigure 24.23 | Headache, blurring of vision, neck rigidity, epistaxis, pain in the shoulder, back and arm, swelling and pain of the heel, difficult labor, epilepsy. |
| 5 | Ren Zhong | Du 26 | A little above the midpoint of the philtrum, near the nostrilsFigure 24.24 | Mental disorders, epilepsy, hysteria, infantile convulsion, coma, apoplexy-faint, trismus, deviation of the mouth and eyes, puffiness of the face, low back pain and stiffness |
| 6 | Yang Ling Quan | GB 34 | In the depression anterior and inferior to the head of the fibulaFigure 24.22 | Hemiplegia, weakness, numbness and pain of the lower extremities, swelling and pain of the knee, beriberi, hypochondriac pain, bitter taste in the mouth, vomiting, jaundice, infantile convulsion |
| 7 | Fei Yang | UB 58 | 7 inch directly above Kun Lun on the posterior border of fibula, about 1 inch inferior and lateral to Cheng Shan (UB 57)Figure 24.23 | Headache, blurring of vision, nasal obstruction, epistaxis, back pain, hemorrhoids, leg weakness |
Type 2: Kidney Deficiency of FBSS:
Patients’ pain demonstrate weakness, and pain at nonspecific-pointed area, difficulty standing, feel better while lying on the bed, the pain is dull and achy, cold in four extremities
Acupuncture points: UB 25 Da Chang Shu, GB 30 Huan Tiao, UB 40 Wei Zhong, UB 60 Kun Lun plus St 36 Zu San Li, Sp 6 San Yin Jiao, and Ki 3 Tai Xi. ( Please see tables 24.1, and 24.2)
Table 24.2
| Points | Meridian/No. | Location | Function/Indication | |
| 1. | Zu San Li | St 36 | On finger-breadth from the anterior crest of the tibia in tibialis anterior muscleFigure 24.22 | Gastric pain, vomiting, hiccup, abdominal distension, diarrhea, dysentery, constipation, mastitis, enteritis, knee joint and leg pain, edema, cough, asthma, waste syndrome, poor digestion, hemiplegia, dizziness, insomnia, mania |
| 2. | San Yin Jiao | Sp 6 | 3 inches directly above the tip of the medial malleolus, on the posterior border of the medial aspect of the tibiaFigure 24.22 | Abdominal pain, distension, diarrhea, dysmenorrheal, irregular menstruation, uterine bleeding, morbid leucorrhea, prolapse of the uterus, sterility, delayed labor, night bed wet, impotence, enuresis, dysuria, edema, hernia, pain in the external genitalia, muscular atrophy, motor impairment, paralysis and leg pain, headache, dizziness and vertigo, insomnia |
| 9 | Tai Xi | Ki 3 | In the depression between the medial malleolus and tendo calcaneus, at the level of the tip of the medial malleous.Figure 24.21 | Sore throat, toothache, deafness, tinnitus, dizziness, spitting of the blood, asthma, thirst, irregular menstruation, insomnia, nocturnal emission, impotence, frequency of micturition, low back pain. |
Type 3: Blood Stagnation of FBSS:
There is sharp, stabbing pain at specific area in the low back and buttock. The pain is very severe, so that nobody could touch the tender area, difficulty bending, sitting and standing, and turning over in the bed.
Acupuncture points: UB 25 Da Chang Shu, GB 30 Huan Tiao, UB 40 Wei Zhong, UB 60 Kun Lun plus Sp 10 Xue Hai, UB 17 Ge Shu, LI 4 He Gu, UB 57 Cheng Shan.
(Please refer to tables 24.1, 24.3)
Table 24.3
| Points | Meridian/No. | Location | Function/Indication | |
| 1 | Xue Hai | Sp 10 | 2 inch above the mediosuperior border of the patella (Knee Cap)Figure 24.21 | Irregular menstruation, dysmenorrheal, uterine bleeding, amenorrhea, urticaria, eczema, erysipelas, pain in the medial aspect of the thigh |
| 2 | Ge Shu | UB 17 | 1.5 inch lateral to the middle line of the body on the back, at the level of the lower border of the spinous process of the 7ththoracic vertebraFigure 24.20 | Vomiting, hiccup,belching,difficulty in swallowing, asthma, cough, spitting of blood, afternoon fever, night sweating, measles |
| 3 | He Gu | LI 4 | On the dorsum of the hand between th e1st and 2nd metacarpal bones, approximately in the middle of the 2ndmetacarpal bone on the radial side.Figure 24.25
|
Headache, pain in the neck, redness swelling and pain of the eye, epistaxis, nasal obstruction , rhinorrhea, toothache, deafness, swelling of the face, sore throat, arotitis, trismus, facial paralysis, febrile dieseases with anhidrosis, hidrosis, abdominal pain, dysentery, constipation, amenorrhea, delayed labour, infantile convulsion, pain, weakness and motor impairment of the upper limbs. |
| 4 | Cheng Shan | UB57 | Directly below the belly of gastrocnemius muscle, on the line joining Wei Zhong UB40 and calcaneus tendon, about 8 inch below Wei Zhong UB40Figure 24.23 | Low back pain, spasm of the gastrocnemius, hemorrhoids, constipation, beriberi. |
TENS is thought to disrupt the pain transmitting to the brain delivering a different, non-painful sensation to the skin around the pain site. In essence, it modulates the way we process the pain sensations from that area, i.e. it closes the pain gate to the brain. It can also trigger the brain to release endorphins. Endorphins act as natural painkillers, and help promote a feeling of well-being.
5. Local Nerve Block
An epidural nerve block is the injection of corticosteroid medication into the epidural space of the spinal column. This space is located between the dura (a membrane surrounding the nerve roots) and the interior surface of the spinal canal formed by the vertebrae.
After a local skin anesthetic is applied to numb the injection site, a spinal needle is inserted into the epidural space under fluoroscopic (x-ray) guidance, using a contrast agent to confirm needle placement. Local anesthetic and corticosteroid anti-inflammatory medication are delivered into the epidural space to shrink the swelling around nerve roots, relieving pressure and pain.
6. Intrathecal Morphine Pump
Pain pump delivery of narcotic drugs is a rather new option available to persons with cancer and non-cancer pain. It is also called intraspinal (within the spine) or intrathecal (within the spinal canal) delivery. It was first used in 1979 after the discovery of narcotic receptors in the spinal cord. The use of an implant device to deliver medications directly in the area of the spinal cord was first used in 1981 for cancer pain. Since then, the pain pump has been used for chronic non-cancer pain such as failed low back surgery syndrome and spasticity from neurological conditions like multiple sclerosis, spinal cord injury, and cerebral palsy.
About Peter’s Treatment:
Peter underwent our treatment with both acupuncture and physical therapy. The typical protocol was as following,
- Peter was first put in the bed with heating pad on the low back for about 10 to 15 mins, his low back muscles were gradually loosening, then massage was given to further relax his low back muscles.
- After massage, acupuncture treatment was given, the most important points were selected based on the above principal. He was given needles with electrical stimulation for 20 to 30 min, his energy flow, therefore, is activated and the pain is gradually decreased.
- He then was transferred to physical therapy area, started to strengthen his abdominal and low back muscles with the above guidance.
- He was given the above treatment for about 20 sessions, he felt greatly improvement after the treatment. He has had more flexibility and much less pain. His pain scale decreased to 2/10 from 10/10. He was pain free for one year, and he sometimes returns to my office for tuning.
Tips for patients who had low back surgery, but still feel a lot of pain on the low back:
- MRI of low back spine is necessary to check any new injuries, such as new herniated disc, degenerative changes of other levels, any loosening of the screws, and spinal stenosis.
- Be very cautious for the subsequent low back surgery. Sometimes, you may be advised to have the second surgery for your low back. From my personal experience, I did not see many successful cases after the secondary even third low back surgery.
- Try to find a physiatrist MD, who also practices acupuncture. Physiatrist MDs are trained in US for Musculoskeleton Medicine. They not only understand your problem but also more specifically treat you with acupuncture. They also could guide your physical therapist for the treatment.
- The combination of physical therapy, massage and acupuncture treatments are very important, because these combined treatments could not only relax your muscles but also maximize your abilities to perform core body strengthen.
- Different patients like different sequence of the treatment, it is not absolutely necessary to have massage, acupuncture, then physical therapy, because everybody is different. It depends on your personal preference. The most important is that you have to have the combined treatment to benefit the most.
- If you drive a distance for longer than 30 min, it is wise to have the lumbosacral corset, i.e. low back brace on, the brace will protect your low back and prevent further injuries.
Tips for acupuncturists:
- You must clearly understand the patient’s pathological mechanism. Some patients are not allowed to have flexion exercise, some patients not for extension exercise.
- Heating pad and massage are very important to induce energy and relax low back muscles.
- LI 4 is a very important point to increase the secretion of endorphin and inhibit the up going reticular formation to send the pain signal to the brain.
- Electrical stimulation on the back points is a must.