News Letter, Vol. 3 (1), January, 2010, © Copyright
Jun Xu, M.D. Lic. Acup., Hong Su, C.M.D., Lic. Acup.
Robert Blizzard III, DPT
Rehabilitation Medicine and Acupuncture Center
1171 East Putnam Avenue, Building 1, 2nd Floor
Greenwich, CT 06878
Tel: (203) 637-7720
Low back pain-spine compression fracture
Collapse of the bone in the spine
www.yanduguke.com
Linda S. is a 70 year old female, who complains of low back pain the day after she bent down to pick up her 1 year old granddaughter. She felt sudden onset low back pain; she had no history of low back pain before. She immediately felt entire low back spasm and was unable to bend forward and move her back. She had difficulty sitting and standing, the only position she felt comfortable was lying on the bed. She called her daughter right away; she was put on bed rest, she thought she might have low back sprain, she would get better after rest on the bed overnight. However, at the second day, she still felt the pain was sharp and stabbing, she could not move. Therefore, she was brought to me for evaluation and treatment.
By inquiry of her pain, she reported her pain was constant, and the pain also felt at the right hip, accompanied with stomach ache, slightly shortness of breath. But there were neither pain radiating down to legs nor urinary nor bowel incontinency; she denied any numbness or tingling sensation. The patient had history osteoporosis for 20 years, she was advised to take vitamin D 400 units and calcium 800 mg per day, forgetting many times to take them. Her daily exercise is swim and stationary bike one or two times per week.
I examed her, she had curved back to the right side of spine, i.e. kyphosis by medical term, her muscles on the right side of back were very spasmodic, however, the muscles on the left side of the back were looser, she looks like to have a hunchback. I was not able to identify a specific spot of her back pain, only at the vague area of entire low back. Also her muscle strength was unable to be checked because of pain. She did not have any abnormal sensation at either leg.
The above signs and symptoms indicated that she might have diagnosis of Spinal Compression Fracture. I immediately ordered CT-scan of her spine, which showed the following,
www.haodf.com
The CT-Scan depicted the wedge shaped vertebra, and confirmed my diagnosis of low back spinal compression fracture.
The Causes of Spine Compression Fracture:
The underline pathophysiology spinal compression fracture is osteoporosis, i.e. the vertebral bones lost their bone substance, the shape of the bones is existed, but the bones can not hold certain weight added to their body. The sponge liked bone at the low back spine can not sustain any acute stress, such as sudden bending forward to tie shoe lace, pick up something from the floor, etc. The reasons for osteoporosis are as following,
1. For women, the leading risk factors are menopause, or estrogen deficiency, cigarette smoking, physical inactivity, use of prednisone and poor nutrition. For men, except all the above nonhormonal factors, low testosterone levels also may be associated with osteoporosis.
2. Renal failure and liver failure, which would make nutritional deficiencies, leading to decreased bone remodeling and increased osteopenia.
3. Genetics, osteoporosis can be observed in closely related family members.
4. Malignance, i.e. malignant tumors, might metastasize to the spine, such as myeloma, lymphoma, renal cell, prostate, breast, lung cancers.
5. Infections: chronic osteomyelitis may result in spinal compression fracture.
The following are the major symptoms of spinal compression fracture:
- Sudden, severe back pain.
- Worsening of pain when standing or walking.
- Loss of height.
- Deformity of the spine – the curved, “hunchback” shape.
- Some pain relief when lying down.
- Difficulty and pain when bending or twisting.
- Neurologic problems may manifest in many ways:
- Reduced leg strength (paresis) or complete weakness (paralysis) is an obvious problem.
- Loss of sensation in the lower extremities and in the perianal area (saddle anesthesia) can be just as important.
- Urinary retention and urinary and fecal incontinence are very important signs that indicate the need for emergency surgery.
Most patients only had the following slight activities, and then the pain starts:
- Slipping on a rug or making a misstep.
- Lifting a suitcase out of the trunk of a car.
- Lifting a bag of groceries.
- Getting up from sitting position
- Bending to the floor to pick something up.
- Lifting the corner of a mattress when changing bed linens.
- Getting in or out of car
Signs of Multiple Spinal Compression Fractures
Some patients might have multiple spinal compression fractures without notices. However, by careful examination, you may find the following,
- Kyphosis (curved back, or hunchback): These fractures often create wedge-shaped vertebral bones, which makes the spine bend forward (Kyphosis). Sometimes, your body might twist the spine to the side leading to Scoliosis. Eventually, neck and back pain may develop as your body tries to adapt the posture changes of the dynamic train of entire spine.
- Height loss: With each fracture of a spinal bone, the spine loses some of its height. Eventually, after several collapsed vertebrae, the person’s shorter stature will be noticeable.
- Hip pain: The shorter spine brings the rib cage closer to the hip bones. If rib and hip bones are rubbing against each other, there will be discomfort and pain.
- Breathing problems: If the spine becomes severely compressed, lungs may not function properly and breathing can be seriously affected, such as shortness of breath, sometimes the poor spine position may make people prone to infection, such as pneumonia or bronchitis.
- Stomach complaints: A shorter spine can compress the stomach, causing a bulging stomach and digestive problems like constipation, poor appetite, acid reflexes, and weight loss.
Treatment of Spinal Compression Fractures
1. The best treatment is prevention. This is best accomplished by treating osteoporosis with exercise, calcium, and medications.
1). Medications for osteoporosis
Calcium 1000 mg per day should be taken for women before menopause and a 1200 mg per day for women who are postmenopausal.
Vitamin D 800 IU for women before menopause and 1000 IU vitamin D for postmenopausal women. Men up to age of 50 should increase vitamin D and calcium intake to 800 IU of vitamin D and 1000 mg of calcium per day.
Bisphosphonates, such as alendronate (Fosamax), ibandronate (Boniva), risedronate (Actonel), and zoledronic acid (Reclast), which slow the rate of bone thinning and can lead to increased bone density. These medicines may be used in men and women.
2). Regular weight bearing exercise. Increased walking, jogging, tai chi, stair climbing, dancing, and tennis. Muscle strengthening exercises include weight training and other resistive exercise. Weight bearing exercise programs not only increase bone density but also improve both heart and lung functional ability and muscle strength. You may walk with a one to three pound of sand bag tied on your each calf for 2 to 3 miles a day, it will greatly improve your bone density if you stick to the program longer enough.
3). For prevention, you should take all preventative procedures such as checking and correcting vision and hearing, evaluating any neurological problems, reviewing any prescription medications for side effects that may affect balance, and providing a check list for improving safety at home. Wearing undergarments with hip pad protectors may protect an individual from injuring the hip in the event of a fall. Hip protectors may be considered for patients who have significant risk factors for falling or for patients who have a previously fractured hip.
4). Avoidance of tobacco use and excessive alcohol intake. Alcohol and cigarettes inhibit osteoblast cell activities and improve osteoclast cell functioning. Osteoclast cells usually destroy the bone density and osteoblast cell build up the bone density.
2. Alleviating the pain: Usually, treatment is aimed at alleviating the pain, and preventing injuries in the future, we use physical therapy, acupuncture, medications, etc.
1). Physical Therapy
Recent research has shown many benefits of using Whole-Body Vibration (WBV) to increase strength and decrease bone mineral density losses from astronauts, athletes to those recovering from injury. Holding a quarter squat position for 30 seconds on a WBV machine set at 50 Hz would be equivalent to performing 1,500 squats without the stress on the joints. WBV is very effective to increase BMD in post-menopausal women even in comparison to a walking regimen (http://www.biomedcentral.com/1471-2474/7/92/, http://www.ncbi.nlm.nih.gov/pubmed/15040822?dopt=AbstractPlus)
Wearing a back brace is a very effective means to prevent unwarranted motions of the spine during early healing. Be cautious of keeping a patient in a brace for an extended period of time typically over 6-8 weeks to avoid secondary complications of immobilization. Maintaining a neutral spine is very important and must be taught how to properly perform functional activities such as getting in and out of bed while keeping the spine straight by using a technique called the “log roll” to go from lying on ones back with knees bent to log rolling to their side then pushing with their upper arm to a seated position and finally to standing.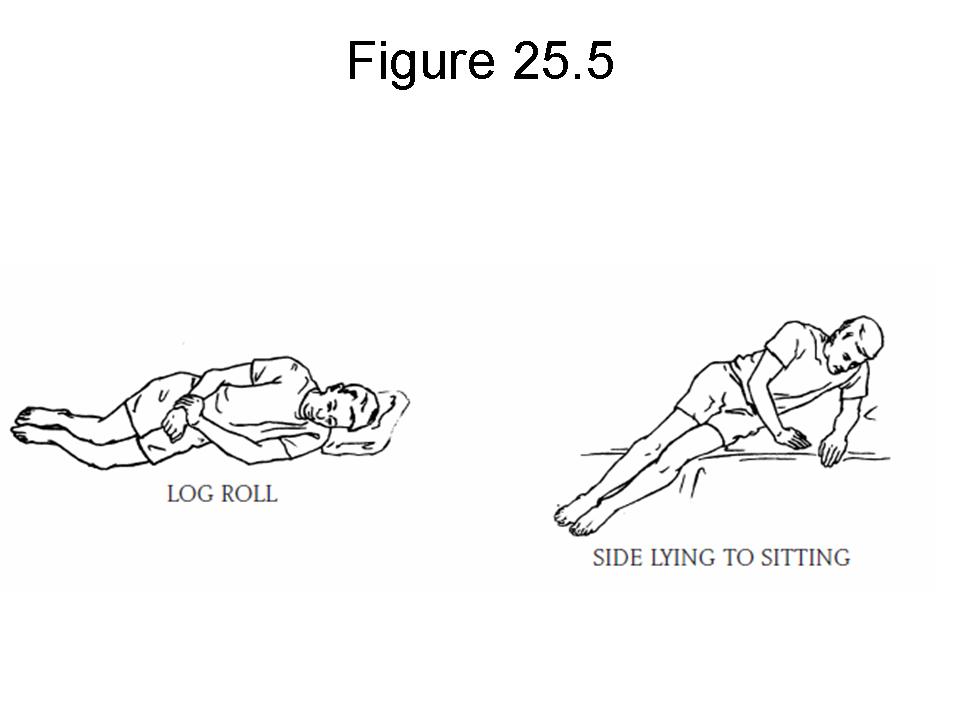
http://www.pvhs.org/documents/Orthopedics/ThorasicSpineSurgery.pdf
In addition to learning how to properly perform activities of daily living such as getting in and out of bed it is very important to work on core stabilizing with exercises such described in the previous newsletter dealing with low back pain with failed back surgery syndrome with link at https://drxuacupuncture.co/2010/12/19/low-back-pain-again-after-back-surgery/
Performing a balance test such as the Berg Balance Test or Tinetti Test will give objective measurement of current balance level and risk of falls. Preventing the risk of falls is very crucial as fractures are more likely with low bone mineral density levels.
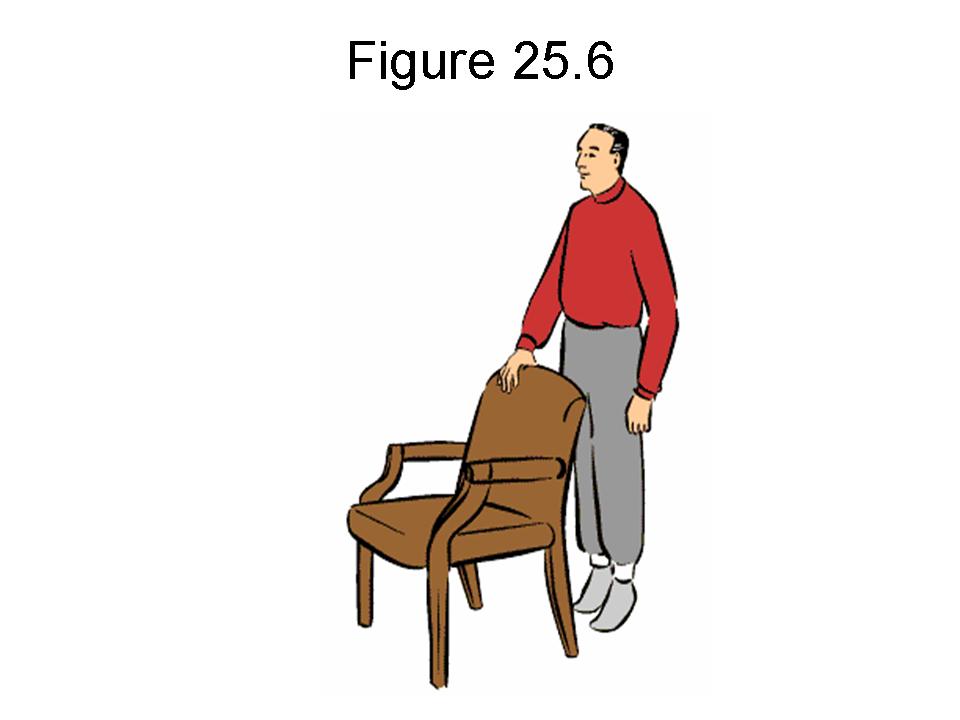
There are many ways to improve balance and progressions to do so. A basic progression would be standing with feet at shoulder width in front of a counter or couch so that you can use your hands to catch yourself if you experience a loss of balance or better yet, have a spotter. Once able to hold that shoulder width stance without loss of balance, take a narrow width stance progressing to your feet being right next to each other for 1 min. Taking a smaller base of support, such as bringing the feet closer, makes the exercise more challenging. From there you can balance on a single leg taking turns between the left and right foot. Next you are ready to try the shoulder width stance with your eyes closed working again to the narrow width stance with eyes closed.
http://www.diabetesmonitor.com/diet-and-lifestyle/exercise/national-institute-of-aging-guidelines/chapter4_balance_plantar.htm
Next, assume a stance where one foot is in front of the other such as a walking stride and again work balance with eyes open then narrowing the stance till one foot is directly in front of the other in a heel to toe fashion called tandem stance. Once able to accomplish tandem stance with eyes open go back to walking stride stance and work to tandem stance with eyes closed.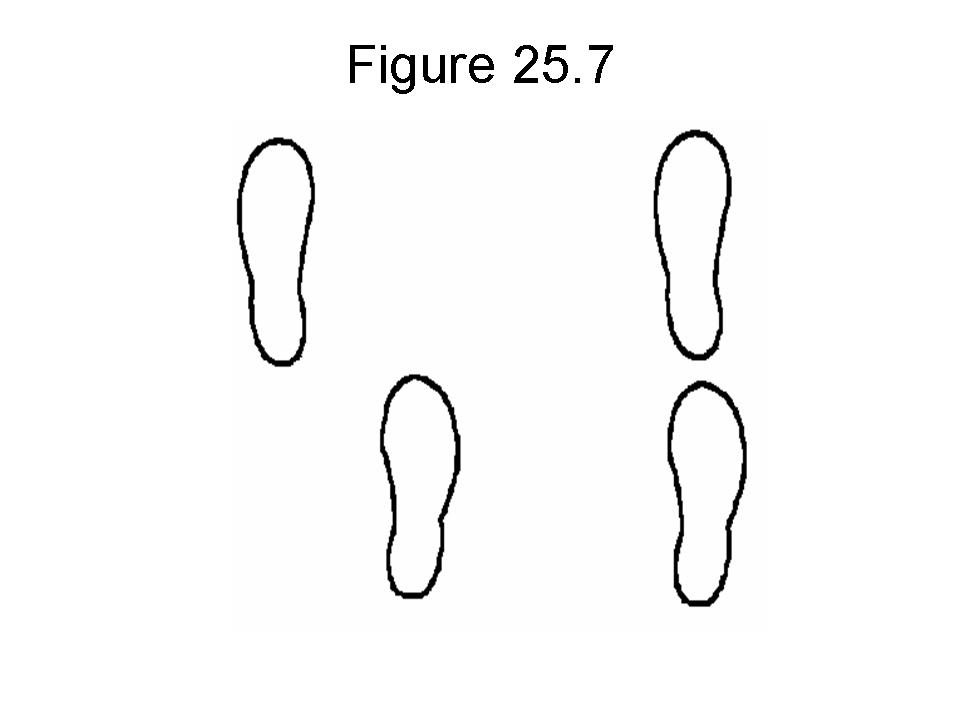
http://www.exercise-to-a-healthier-life.com/tandem-stands.html
Another way to progress with balance exercises is to go from a flat stable surface such as the ground to an unstable surface such as a balance board or foam pad. An unstable surface will increase muscle activity in the ankles, knees, hips and core making the exercise more challenging.
http://www.physicalcompany.co.uk/products/product_detail.asp?productId=ABPE
In addition to performing core and balance exercises, it is important to increase the strength in the upper spine and shoulders. Using a theraband is easy but more importantly effective for increasing muscle strength. A series of Lat Rows, Lat Pulls, and Shoulder External Rotations are three effective exercises to be performed 3-4 x week for 3 sets of 10, progressing to 2 sets of 15 and finally 1 set of 30 in a row. Start off with a lighter theraband and work you way up to a higher resistance theraband such as progressing through yellow, red, green, blue to black.
http://www.thera-band.com/store/products.php?ProductID=28 Standing Row with Theraband http://www.health24.com/fitness/Exercises/16-1339-1344,33165.asp
Standing Row with Theraband http://www.health24.com/fitness/Exercises/16-1339-1344,33165.asp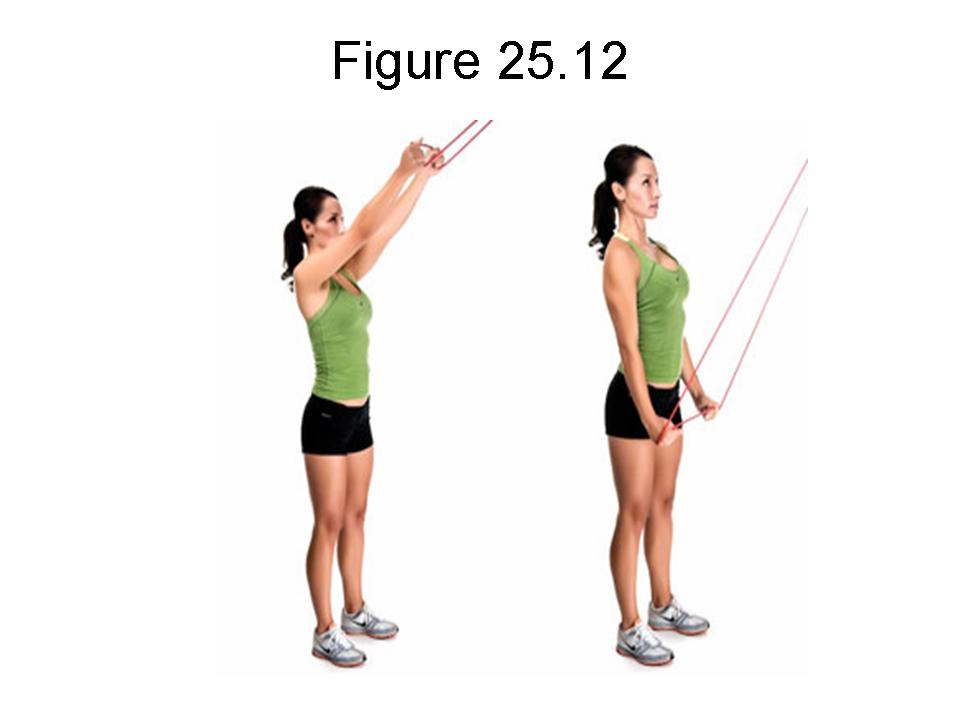
Standing Lat Pulls with Theraband http://www.sbortho.com/educational_resources/strength_exercises.html
External Rotation with Theraband http://www.health.com/health/library/mdp/0,,zm2387,00.html
2). Acupuncture
Hua Tuo Jia Ji points are sets of specially designed points used to treat spine disease. By palpation, you should feel the tender points around the spinal process, then insert the needles into the disc about 0.5 inch deep and one up and one lower levels of the spinal process, plus 0.5 inch of the lateral sides of the three levels, i.e. total 9 needles inserted into the tender points around the spine and adjacent area.
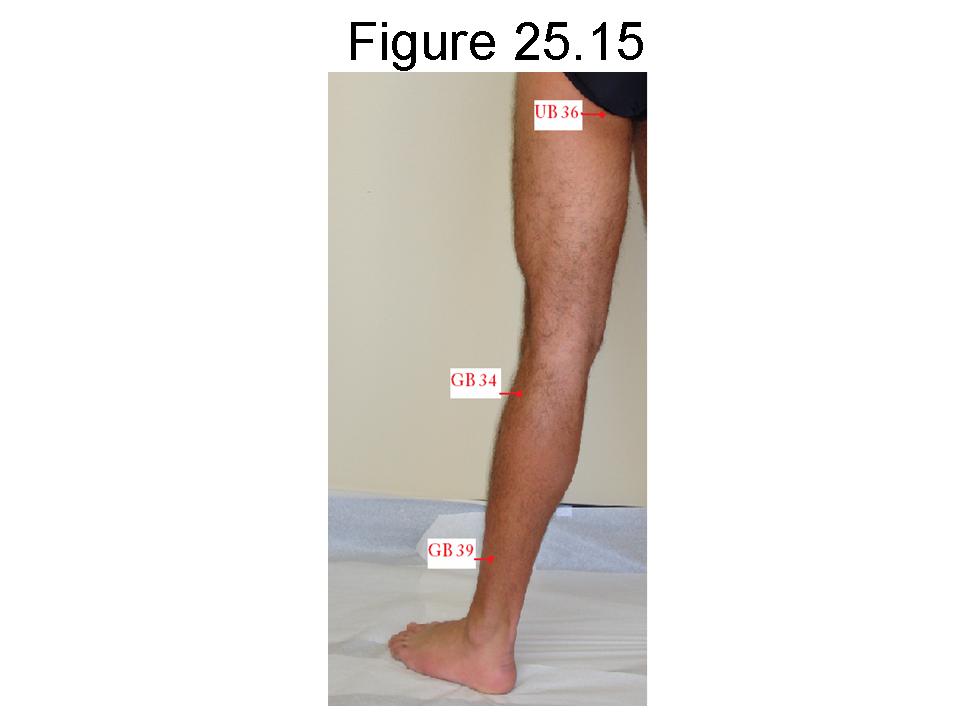
I also selected the following points: Sheng Shu, Qi Hai Shu, Chi Bian, Huan Tiao, Yang Ling Quan, Fei Yang, Ju Liao, Jue Gu, and Cheng Fu.
Table 25-1
| Points | Meridan/No. | Location | Function/Indication | |
| 1 | Hua Tuo Jia Ji | ExperiencedPoints | Along the spine, use the most painful vertebral spinal as midpoint, then locate the upper and lower spinal process and 0.5 inch on the either side, you may choose two spinal process as the starting points. See Pic 4-1 | Specifically treat for local neck and low back pain, and pain along the spine. |
| 2 | Sheng Shu | UB 23 | 1.5 inch lateral to midline of spine at the level of the lower border of the spinous process of the second lumbar vertebrta | Nocturnal emission, impotence, enuresis, irregular menstruation, leucorrhea, low back pain, weakness of the knee, blurring of vision, dizziness, tinnitus, deafness, edema, asthma, diarrhea |
| 3 | Qi Hai Shu | UB 24 | 1.5 inch lateral to midline of spine at the level of the lower border of the spinous process of the third lumbar vertebra | Low back pain, irregular menstruation, dysmenorrheal, asthma |
| 4 | Zhi Bian | UB 54 | Lateral to the hiatus of the sacrum, 3 inch lateral to the midline of spine | Pain in the lumbosacral region, muscular atrophy, motor impairment of the lower extremities, dysuria, swelling around external genitalia, hemorrhoids, constipation |
| 5 | Huan Tiao | GB 30 | At the junction of the lateral 1/3 between the great trochanter and the hiatus of the sacrum. | Pain of h elumbar regiin and the thigh, muscular atrophy of the lower limbs, hemiplegia |
| 6 | Yang Ling Quan | GB 34 | In the depression anterior and inferior to the head of the fibula | Hemiplegia, weakness, numbness and pain of the knee, beriberi, hypochondriac pain, bitter taste in the mouth, vomiting, jaundice, infantile, convulsion |
| 7 | Jue Gu( Xuan Zhong) | GB 39 | 3 inch above the tip of the external malleolus, in the depression between the posterior border of the fibula and the tendons of peronaeus longus and brevis | Apoplexy, hemiplegia, pain of the neck, abdominal distension, pain in the hypochondriac region, muscular arophy of the lower limbs, spastic pain fo the leg, beriberi |
| 8 | Cheng Fu | UB 36 | In the middle of the transverse gluteal fold | Pain in the lower back and gluteal regioin, constipation, muscular atrophy, pain, numbness and motor impairment of the lower extremities |
3). Pain Medicines
Pain medications. A carefully prescribed “cocktail” of pain medications can relieve bone-on-bone, muscle, and nerve pain, explains F. Todd Wetzel, MD, professor of orthopaedics and neurosurgery at Temple University School of Medicine in Philadelphia. “If it’s prescribed correctly, you can reduce doses of the individual drugs in the cocktail.”
Over-the-counter pain medications are often sufficient in relieving pain. Two types of non-prescription medications — acetaminophen and non-steroidal anti-inflammatory drugs (NSAIDs) — are recommended. Narcotic pain medications and muscle relaxants are often prescribed for short periods of time, since there is risk of addiction. Antidepressants can also help relieve nerve-related pain.
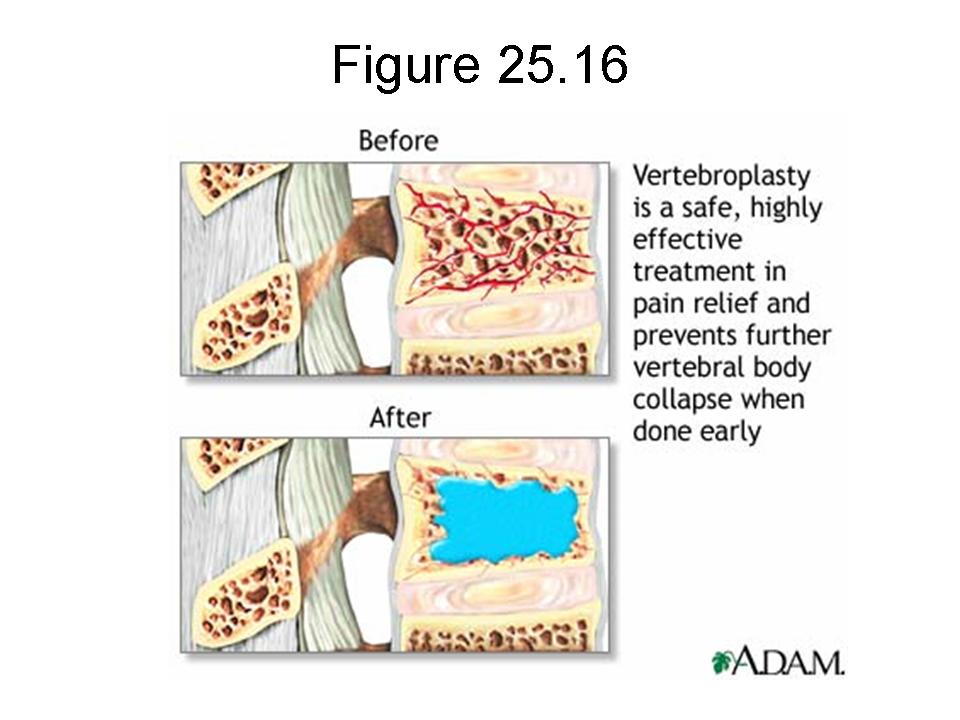
If the pain is severe, and collapse is becoming problematic, procedures called vertebroplasty or kyphoplasty may be considered. In these procedures an interventional radiologist restores the height of the bone and injects cement into the vertebra to stabilize the fracture and prevent further collapse.
Surgical Treatment for Spinal Compression Fractures
When chronic pain from a spinal compression fracture persists despite rest, activity modification, back bracing, and pain medication, surgery is the next step. Surgical procedures used to treat spinal fractures are:
Figure 25.16
From: https://www.healthbase.com
After general anesthesia, or simply under sedation, a special bone needle will be inserted into the soft tissues of the back guided by x-ray, along with a small amount of x-ray dye, which will allow the position of the needle to be seen at all times. Then, a small amount of orthopedic cement, called polymethylmethacrylate (PMMA) will be pushed through the needle into the vertebral body, then the cement will be solid after a few mins. The cement will be filled in the fractured vertebrae, and sustained the body weight over night. Each vertebral body is injected on both the right and left sides, just off the midline of the back.
The cement is sometimes mixed with an antibiotic to reduce the risk of infection, and a powder containing barium or tantalum, which allows it to be seen on the x-ray.
Within a few hours, patients are up and moving around. Most go home the same day.
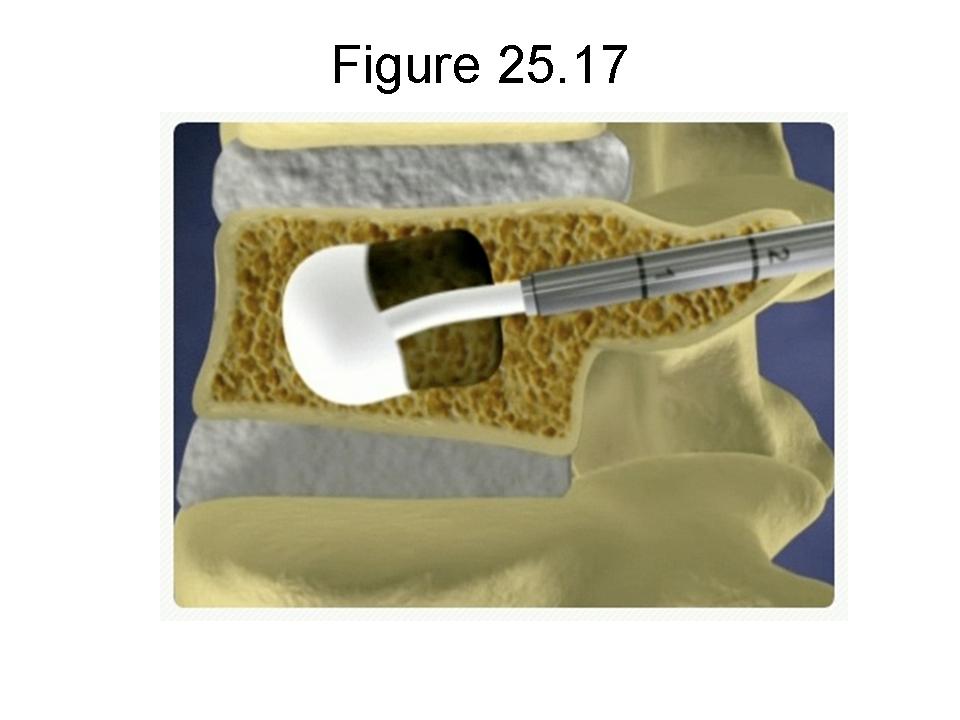
From: www. sarasotaspine.com
Similar to vertebroplasty, Kyphoplasty is performed under local or general anesthesia. Using image guidance x-rays, two small incisions are made and a probe is placed into the vertebral space where the fracture is located. The bone is drilled and a balloon, called a bone tamp, is inserted on each side. These balloons are then inflated with contrast medium (to be seen using image guidance x-rays) until they expand to the desired height and removed. The balloon does not remain in the patient. It simply creates a cavity for the cement and also helps expand the compressed bone.
The spaces created by the balloons are then filled with PMMA, the same orthopaedic cement used in vertebroplasty, binding the fracture. The cement hardens quickly, providing strength and stability to the vertebra, restoring height, and relieving pain.
The above procedures provide new options for compression fractures and are designed to relieve pain, reduce and stabilize fractures, reduce spinal deformity, and stop the “downward spiral” of untreated osteoporosis. In my experience, many patients reported miracle results after the procedures.
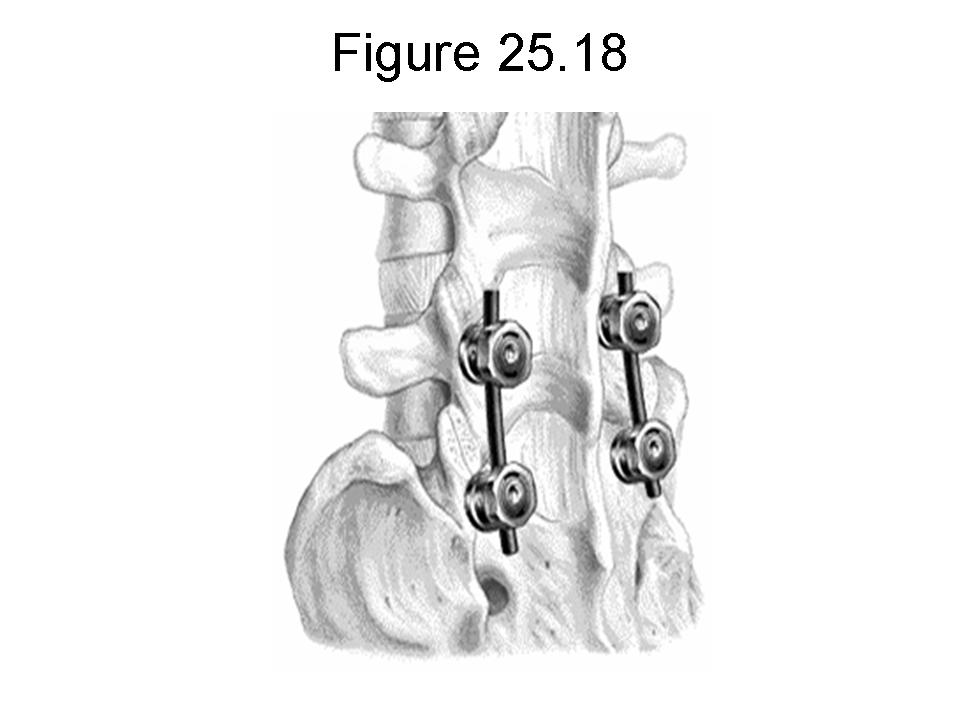
From: http://www.neurosurgery.ufl.edu/
This procedure is used primarily to fuse or immobilize two or more vertebrae and to eliminate the pain caused by abnormal motion of the vertebrae. Supplementary bone tissue, either from the patient (autograft) or a donor (allograft), is used in conjunction with the body’s natural bone growth (osteoblastic) processes to fuse the vertebrae.
The above procedures may help you a lot with a decrease of pain, and improve your spine stability and flexibility. However, the procedures may not solve all your problems. Sometimes, you may feel very much pain after the procedures. Therefore, it is necessary to have acupuncture treatment in order to reduce the pain.
TREATMENT OF LINDA
Linda first underwent physical therapy 2x per week for 4 weeks in another physical therapy facility, she underwent many trunk forward bending and backward extension exercises, however, she felt more pain on the low back after her physical therapy. I did CT scan again, I found out her low back compression fracture was worse than the first CT scan. I immediately informed her stop doing the forward bending exercise, because this exercise causes the further compression fracture.
She was referred to interventional radiology for veterbroplasty treatment. She felt much better after the surgery. However, after 2 months of the surgery, she complained of low back pain again. She came to me for treatment again.
I then started her with physical therapy 2x per week for another 4 weeks and in the mean time, acupuncture treatment 2x per week for 4 weeks, Fosamax also was prescribed for her long term use. After about 6 weeks treatment, her pain is much subsided and she is more flexible.
Tips for the patients:
-
-
- You must give up the bending forward exercise of low back, and try to avoid bending forward postures, for example, do not pick up heavy object from floor, tight your shoes, etc.
- You must check your BMD (Bone Mineral Density) measurements at spine, hip, or forearm by DXA devices.
- Please read my news letter article no. 4, which will give you the information about how to take care of osteoporosis, please see the attached link: https://drxuacupuncture.co/2009/04/27/case-discussion-4/.
-
Tips for the acupuncture practitioners :
1. Acupuncture could decrease the pain, but it can not change the shape of the compression fractured spinal spine.
2. Do not advise the patients not go to the surgery, because the surgery might be the necessity for the treatment of long run.
3. Teach the patients that do not bend their low back forward, which will worse the low back compression fracture. The patient should avoid the bending forward exercise.
4. The patients should be advised to wear lumbar sacral brace to protect the low back during acute stage of the low back pain.
5. Acupuncture is not the only treatment for spinal compression fracture, an integrated treatment might get better results.







4 comments
Jane R Cutts
May 29, 2011 at 5:48 am
I read in this article that Cissus helps in faster bone recovery – http://www.squidoo.com/bonefracturetreatments
Can you guide me if this herb can really make me recover faster from my bone fracture?
nootropics
April 18, 2012 at 9:53 pm
I like your intriguing words. first class stuff. I hope you release many. I will continue watching
best ways to lose belly fat fast
December 24, 2012 at 7:33 pm
Thanks for sharing your thoughts about lose stubborn belly fat.
Regards
Pingback: Acupuncture Back Pain Works