News Letter, Vol. 3 (7), July, 2011, © Copyright
Jun Xu, M.D. Lic. Acup., Hong Su, C.M.D., Lic. Acup.
Robert Blizzard III, DPT
www.drxuacupuncture.co
Rehabilitation Medicine and Acupuncture Center
1171 East Putnam Avenue, Building 1, 2nd Floor
Greenwich, CT 06878
Tel: (203) 637-7720
Shin Splint
http://www.fitnessinformation.net/how-to-heal-shin-splints-ouch
George F is a 16 years old squash player. He’s had a personal coach working with him 4-5 hours of training everyday. The intensive training started when he was 8 years old, and made him one of the top players in US. One day, he complained of right lower leg pain with swelling at the right frontal lower leg. These symptoms happened often, and George’s coach put some ice on it, and asked him to stop training for one day. However, the above treatment did not make him feel any better, and he forced himself to go back for the training. But the pain was getting worse and becoming a constant dull pain with pressure sensation. The pain usually felt worse at the start of exercise and slowly subsided as the exercise continued. When he rested, he felt some relief. The pain often returned after prolonged activity and usually worse in the next morning. He had difficulty jumping, running and even walking, therefore, his mom brought him to me for evaluation and treatment.
By physical examination, there was tenderness at right frontal medial lower leg behind and along the shin bone with slight redness and swelling. The pain spread through the entire right medial shin bone, worse at the lower half of the shin. The lower leg was slightly warm. The pain was worse when I bent his toes and foot downward. George walked with a short stance at the right leg, and leaned to right. He had no knee, hip or low back pain. I ordered X-ray of right leg, which showed no fracture at right tibia and fibular bones. Based on the above, my impression is shin splints, i.e. medial tibial stress syndrome.
Shin Splints is a loose term describing different injuries around lower leg.
The term “shin splints” refers to pain along or just behind the shinbone (tibia) — the large bone in the front of your lower leg. There are two bones in your lower leg. The main bone is called Tibia, i.e. Shin, which hold the stress from your body upon impact from walking, running, etc., the small bone is called fibula, which attaches and stabilizes the muscles around the tibia.
The lower leg is divided into three fascial compartments-anterior, lateral, and postieror-by three membranes, i.e. the anterior and posterior intermuscular septa and the interosseous membrane. Because the septa forming the boundaries of the leg compartments are strong, trauma to muscles in the compartments may produce hemorrhage, edema and inflammation of the muscles. With arterial bleeding, the pressure may reach levels high enough to compress structures in the compartments, which will cause extreme pain called “compartment syndrome”. For severe cases of compartment syndrome, the only treatment is fasciotomy (incision of a fascial septum) to relieve the pressure in the compartments concerned.
Fig. 7.2
hughston.com
Shin splints-edema and pain in the area of the distal two-thirds of the tibia-results from repetitive microtrauma of the tibialis anerior and small tears in the periosteum covering the body of the tibia. Muscles in the anterior compartment swell from sudden overuse, and the edema and muscle-tendon inflammation reduce the blood flow to the muscles. Shin splints are a mild form of the anterior compartment syndrome.
Many athletes have shin splints, such as long distance runners, dancers, tennis, basketball, and football players. etc. There are two predetermined conditions, which will make any athletes prone to have shin splints.
1. High impact and constant stress on your shin, i.e. lower leg’s muscles and bone. This is the key contributor. If you are a sedentary person, you only walk a short distance without any high impact on your leg for your life, you will not have any symptoms of shin splints. However, if you suddenly start to exercise without warm up, or if you have constant, high impact pressure on your leg, it will lead to different types of shin splints.
2. Overpronation or “ Flat Feet”. Many people have flat feet without an arch. This anatomical deficiency changes the dynamic chain from your trunk, hips, knees, ankles and feet. Thus putting tremendous stress on your shins, you may develop shin splints. Inappropriate footwear, such as high heel shoes, as the same token, will change the dynamic chain, and over stretch the muscles and tendons around your shin and cause pain and shin splints.
The high impact and changed dynamic chain make the following symptoms or diseases possible:
• Medial tibial stress syndrome: i.e. the tendonitis and tibial periostitis with Irritated and swollen muscles, often caused by overuse.
• Stress fractures, which are tiny, hairline breaks in the lower leg bones.
• Compartment syndrome, as described above.
Diagnosis of Shin Splints
1. Medical history: As we mentioned before, if you have history of lower leg pain and swelling, warm along the anterior and posterior your shin bone after excessive impact of exercise on your leg without warming up, and if you have pronated feet, you might have the symptoms of shin splints.
2. X-ray: we usually order x-ray to rule out the stress fractures, i.e. to look at if you have a tiny, hairline fracture in your tibia bone.
3. It usually is not necessary to have MRI for the diagnosis of shin splints.
In mild cases, you should treat yourself with the following steps:
• Rest. Avoid high impact activities that cause pain, swelling or discomfort, try low-impact exercises, such as swimming, bicycling or water running.
• Ice massages the affected area. Apply ice packs wrapped with a thin towel to the affected shin for 15 to 20 minutes at a time, four to eight times a day for at least one to two weeks.
• Elevation of your leg: Elevate your affected leg above the level of your heart while you are sitting and sleeping, especially during night.
• Anti-inflammatory drugs. Such as ibuprofen (Advil, Motrin, others), naproxen sodium (Aleve, others) or acetaminophen (Tylenol, others) to reduce pain.
• Wrap your shin with bandage to protect it from swelling further. You should wrap and check it periodically for every a few hours, if the swelling increases, or more pain, or numbness and tingling sensation happens, you should unwrap it right away.
• Wear proper shoes. You should wear a pair of shoe with enough space suited for your foot type, stride and particular sport. If it is necessary you should ask your podiatry or physiatry physicians for recommendation.
• Consider arch supports and appropriate shoe insole. Arch supports and shoe insole can help cushion and disperse stress on your shinbones
In moderate cases, you may need the following treatment:
1. Physical Therapy
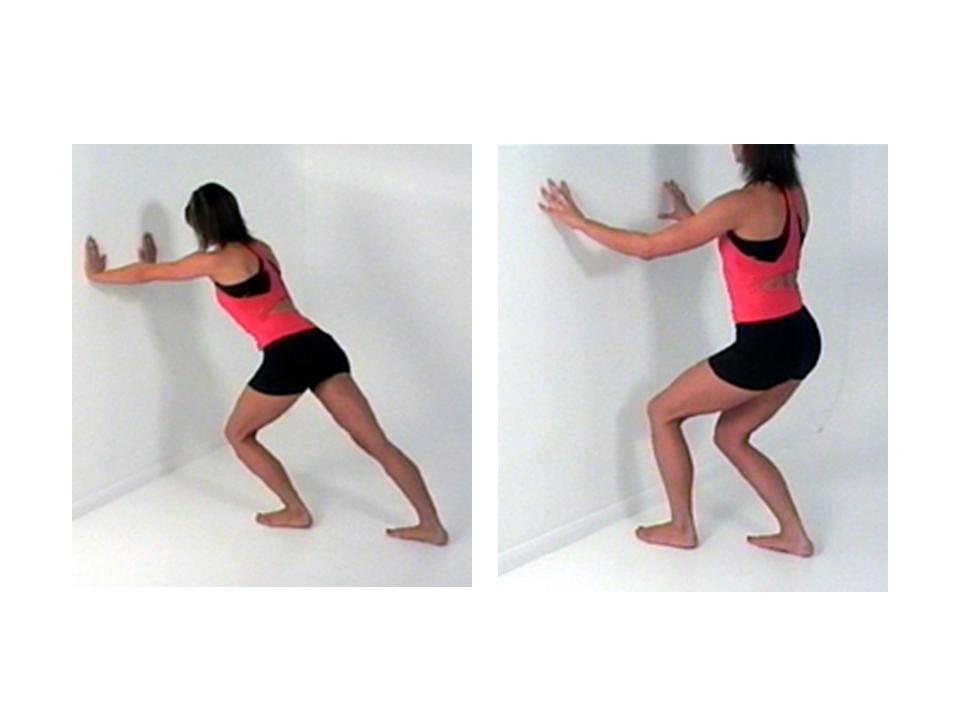
Stretches for the lower leg muscles include calf stretches. Maintaining a straight back leg will emphasis the gastrocnemius and then with a bent back leg shift the target to the soleus muscle. The back ankle should be held on the ground with toes pointing straight forward, each stretch should be held for 30-60 seconds.
Fig 7.3
http://www.sportsinjuryclinic.net/cybertherapist/back/achilles/tendinitis/stretching.php
A stretch for the lower leg muscle on the front of the shin, anterior tibialias, can be performed standing or kneeling as shown below with each stretch held for 60 seconds
Fig 7.4
http://www.teachpe.com/stretching/standing_shin.php
Kinesio Taping is effective to help reduce stress associated with shin splints along with many other physical ailments. There are many varying methods with taping, but the basic theory is to reduce stress through the painful area while activating the proper muscle groups.
Fig 7.5
http://sportsmedinfo.net/kinesiology-taping/234-kinesio-tape-shin-splints
Compression Sleeves have also been effective in reducing fatigue and decreasing soreness associated with shin splints when wore while running. Some pairs allow for ice packs to be held in place post activity to speed up recovery and reduce inflammation.
Fig 7.6
http://www.return2fitness.net/Supports_and_Braces/Shin_and_Calf_Supports/mueller-shinsplint
http://revelsports.com/Zensah/6055_Zensah_Compression_Sleeves_Calf_Shin_split.asp
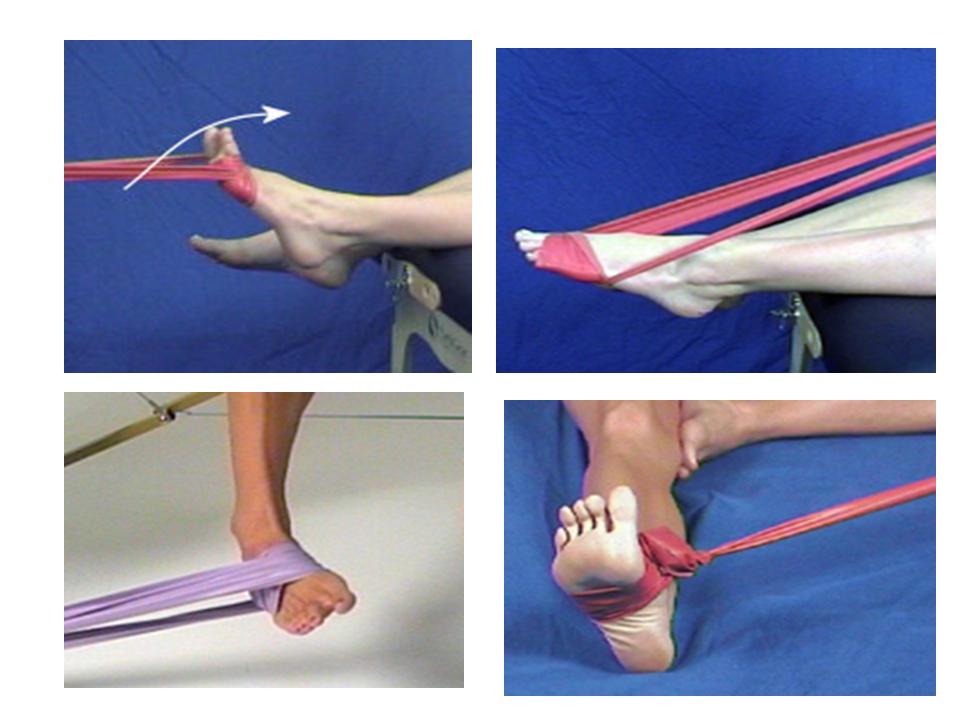
Strengthening the muscles of the ankle and lower leg is important to prevent imbalances in the lower leg. The exercises should be able to be performed for 20-30 reps painfree before adding resistance from a Thera-Band as demonstrated below. The patient should build up to 3 sets of 10 reps for each exercise. These exercises are referred to as 4-way Ankle Exercises. The first motion in DorsiFlexion as the foot is pulled back towards the body as resistance is applied in the opposite direction. The next motion is PlantarFlexion as the foot is pushed down away from the body against resistance. The third motion is Inversion as the foot is turned down and in against the Thera-Band. The final motion is Eversion as the foot is turned up and out.
Fig 7.7
http://www.sportsinjuryclinic.net/cybertherapist/front/ankle/broken_ankle/rehabilitation.php
2. Acupuncture: I usually chose the following acupuncture points, both side LI 4 He Gu, LI 11 Qu Chi,
Then depends on which compartments, I chose different group,
For anterior and lateral compartments:
Sp 6 San Ying Jiao, Sp 7 Lou Gu, Sp 8 Di Ji, Sp 9 Ying Ling Quan, Sp 10 Xue Hai, Sp 11 Ji Men, St 36 Zu San Li, St 37 Shang Ju Xu, St 39 Xia Ju Xu.
Fig 7.8
For posterior compartment:
UB 55 He Yang, UB 56 Cheng Jing, UB 57 Cheng San, UB 59 Fu Yang,
Fig 7.9
re cases, i.e. the real compartment syndrome, you may need surgery, i.e. fasciotomy (incision of a fascial septum) to reduce the increased pressure inside the specific compartment.
Fig 7.10
catalog.nucleusinc.com
George’s treatment:
George was asked to stop playing squash immediately. He was advised to have ice massage 10 min on right shin for 4 to 5 times a day for 2 weeks to reduce his inflammation. Acupuncture treatment was performed 3x per week for 4 weeks accompanied with physical therapy. After treatments his right shin splints was much better. He returned to squash training after 2 months.
Tips for patients:
1. If you have flat feet, please try to use a pair of arch support, which will help you to prevent shin splints from occurring.
2. Warm up 15 min before you go to any high impact sports, such as running, tennis, jumping, martial arts, etc.
3. Always ice massage your shin bone 10 to 15 min after your high impact sports, even you only have slightly pain at your shin bone.
4. Prevention is better than treatment!
Tips for Acupuncture Practitioners:
1. Always teach your patients for self care, such as ice massage, arch support and appropriate foot wear for high impact sports. They have to change their shoe if they run long distance every 350 miles.
2. Acupuncture treatment accompanied electrical stimulation about 30 min will get the best results.
3. You should not use moxbustion for the patients.
4. For severe compartment syndrome: If you could not feel pulse at the patient’s feet, you must send the patient to surgeon ASAP. The leg might be saved if the patient has fasciotomy within a few hours.











3 comments
Raj Chopra
January 24, 2013 at 10:59 am
I suffer with anterior shin splints and have recently acquired a bactch of acupuncture needles.
I have used them a couple of times but did not get the relief I expected. maybe because I inserted only one needle into each shin and inserted them into the diect pain area.
Is there a better place to insert the needles?
Also should I be inserting more?
Hi, Raj,
You should follow the points I indicated and try them.
Best,
Jun Xu, MD
drxuacupuncture
January 25, 2013 at 8:56 pm
Hi, Raj,
You you use the points I indicated and try them. I am pretty sure you will feel better.
Best,
Jun Xu, MD
Daryl
January 10, 2015 at 3:12 pm
Thanks for one’s marvelous posting! I certainly enjoyed reading it, you will
be a great author. I will ensure that I bookmark your blog and may come back someday.
I want to encourage you to definitely continue your great
writing, have a nice holiday weekend!